Volume 71, Issue 2 (April 2022)
Review Series: Linking Drug-Allergy and Autoimmune Diseases
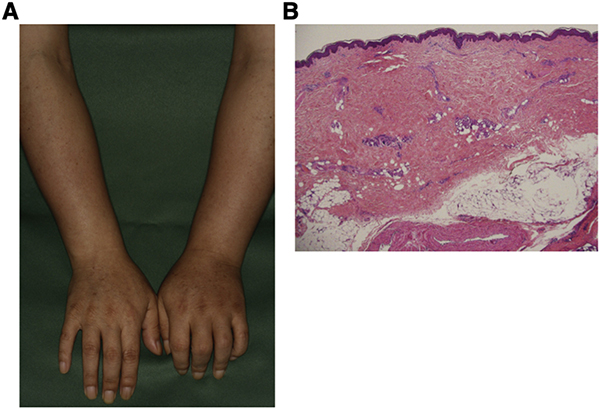
Hamaguchi provides a comprehensive review of drug-induced scleroderma-like lesions, including frequency, causative drugs, mechanisms, clinical features and comparison with systemic sclerosis (SSc). A wide variety of drugs can cause scleroderma-like lesions, including chemotherapeutics. Unlike SSc, most cases are negative for autoantibodies, have no vascular abnormalities, and seem to have minimal organ damage. In recent years, however, there has been an increasing number of reports of scleroderma-like lesions due to immune checkpoint inhibitor (ICI), including cases in which patients with pre-existing SSc had their organ involvement worsened by induction of ICI.
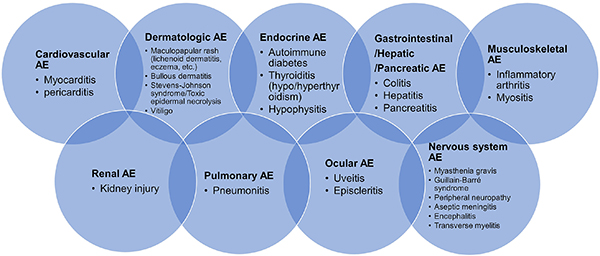
Okiyama and Tanaka offer an excellent review of ICI-induced irAE, including its epidemiology, risk factors, clinical phenotypes of cutaneous irAE, and management. While the activation of CD8+ T cells by ICI is important for the original purpose of cancer immunity, CD8+ T as well as B cells are also involved in irAE. In addition, cytokines and microbiomes associated with the development of irAEs have also been reported. Further studies may identify risk factors, biomarkers, and appropriate treatments as well as prevention of irAEs without loss of cancer immunity by ICI.
Watanabe and Yamaguchi's review article focuses on the association between drug allergy and autoimmune diseases. The high frequency of drug eruptions in patients with SS, SLE, and adult-onset Still's disease is comprehensively reviewed. Intriguing observations include the development of SS-like symptoms after SJS/TEN onset and the high prevalence of anti–SS–A antibodies in SJS/TEN. SLE is a known risk factor for SJS/TEN, but both may involve common pathologies such as excessive immune responses, dysregulated regulatory T cell function, and neutrophil extracellular traps.
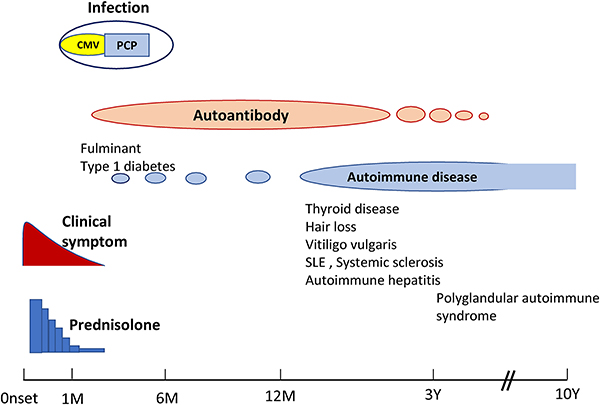
Sueki et al. give us an intriguing review focusing on the relationship between the immune mechanism of non-HIV IRIS and drug allergies. The pathophysiology of non-HIV IRIS can be recognized in several disorders treated with corticosteroids, immunosuppressants, molecular-targeted drugs, TNF-α antibody drugs, immune checkpoint inhibitors, and dipeptidyl peptidase-4 inhibitors. They describe the concept and draft the diagnostic criteria of non-HIV IRIS, comprehensively reviewing DIHS/DRESS, SJS/TEN, DPP4 inhibitor-related bullous pemphigoid, and irAE as events associated with non-HIV IRIS. This interesting field awaits the development of biomarkers that can help diagnose and predict the development of IRIS.