Volume 74, Issue 1 (January 2025)
Editor's Choice
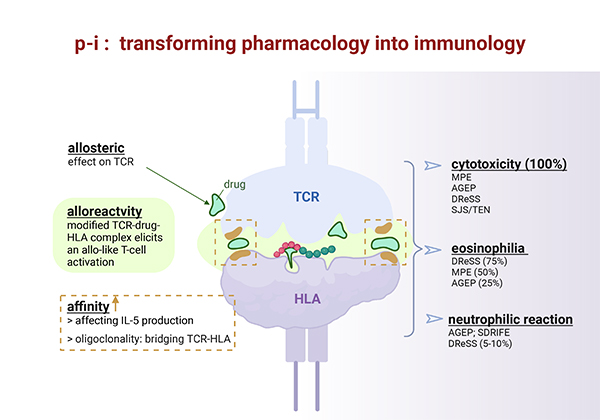
Editor’s comment: Pharmacological interaction with immune receptors (p-i) is a mechanism that explains one type of drug hypersensitivity reaction (DHR). A drug binds to immune receptors, such as HLA or T cell receptor (TCR), causing T cell activation and leading to inflammatory manifestations such as exanthems, eosinophilia, and Steven-Johnson syndrome. Understanding p-i theory is important for preventing and treating DHRs, and it may also help to understand TCR signaling and alloreactivity. Dr. Werner J. Pichler, who proposed the theory, provides us with a comprehensive review.
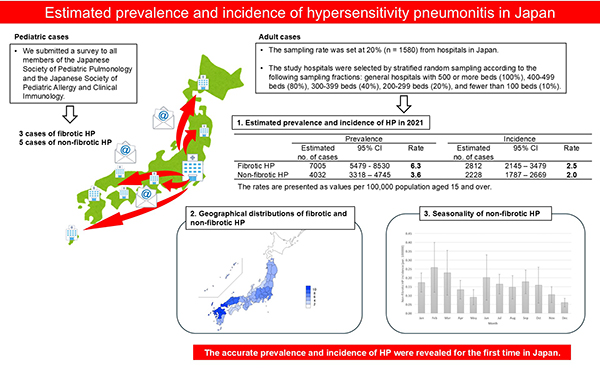
Editor’s comment: The latest guidelines on hypersensitivity pneumonitis (HP) categorize the disease as either fibrotic or non-fibrotic, due to the greater clinical utility of this classification. However, little has been known about the exact prevalence and incidence of fibrotic and non-fibrotic HP in Japan. Okamoto et al. report, for 2021, the number of patients with fibrotic or non-fibrotic HP who visited the hospital and the number of newly diagnosed cases of fibrotic or non-fibrotic HP in Japan. This is the first study shed light on the prevalence and incidence of fibrotic and non-fibrotic HP in Japan.
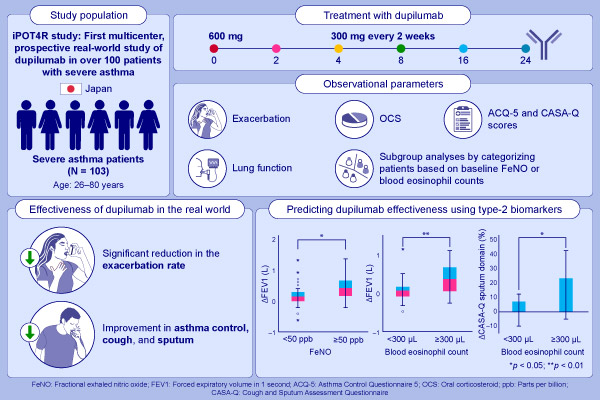
Editor’s comment: Dupilumab, a human monoclonal antibody against IL-4R, decreases the occurrence of exacerbation events and improves pulmonary function in severe uncontrolled asthma. Mizumura et al. conducted a multicenter, prospective study in real-world settings to confirm the efficacy of dupilumab in improving FEV1 and sputum symptoms in a Japanese population. The information that both increased blood eosinophils and high FeNO can be predictive markers of the efficacy may help clinicians decide when to introduce dupilumab to patients with severe asthma with type 2 inflammation.